
Every year, diseases of the musculoskeletal system worry more and more people, and their development at a young age is increasingly being observed. This is facilitated not only by changes in lifestyle, but also by increased levels of injuries, which are largely interrelated. One of the most common pathologies of the musculoskeletal system is arthrosis of the hip joint, which is characterized by the occurrence of progressive pain and limited mobility. Eventually, the disease can lead to complete joint disability and disability. To avoid the occurrence of unwanted consequences, it is important to start arthrosis treatment as early as possible. And if in the early stages of development it can be stopped by conservative methods, then in the event of severe changes, it is possible to restore the function of the hip joint and get rid of unbearable pain only with the help of high -tech surgery.
Is arthrosis of the hip joint
Arthrosis of the hip joint is a chronic degenerative-dystrophic disease in which the gradual destruction of the hip joint occurs. At the same time, all its components are gradually involved in pathological processes, but hyaline cartilage is particularly affected, which leads to narrowing of the joint space and deformation of other components. More often, pathological changes occur in only one hip joint, although both can also be affected simultaneously.
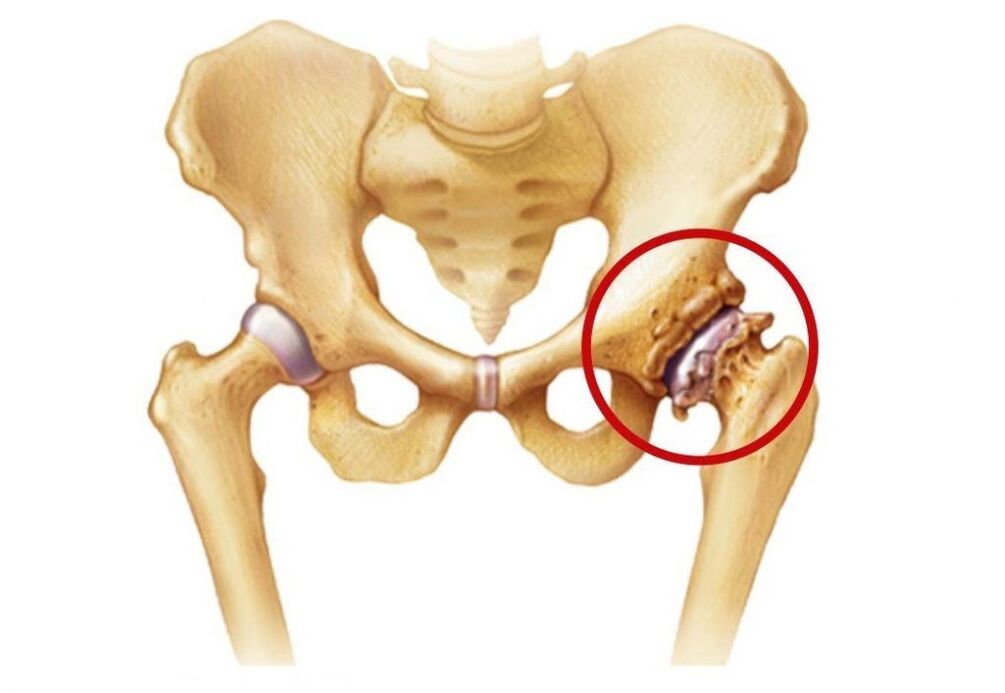
The hip joint is the largest in the human body, as it bears the greatest load during the day. Each of them is formed by the head of the femur and the acetabulum, which is a bowl -shaped indentation in the pelvis. Both surfaces are covered with smooth and moderately elastic hyaline cartilage. He is the one who ensures smoothness and unobstructed sliding of the femoral head in natural depression and thus makes it possible to make movements in various planes.
The movement of the hip joint is provided by a group of muscles connected to it by fasciae. It is also surrounded by ligaments, its job is to limit its mobility within physiological limits and ensure the stability of its position.
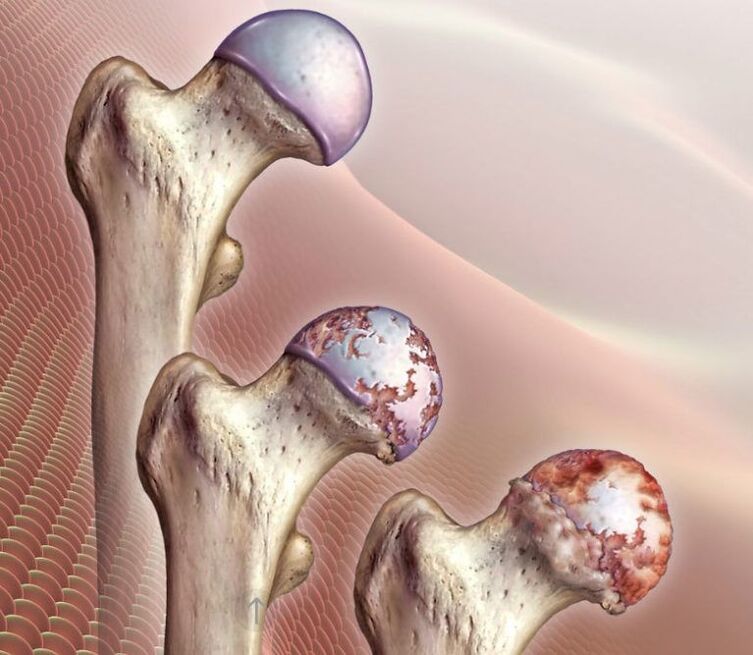
The entire joint is surrounded by an articular capsule covered with a synovial membrane. Its main task is the synthesis of synovial fluid, which lubricates the adjacent part of the hip joint and at the same time acts as a carrier of nutrients for it. It is from the synovial fluid that the hyaline cartilage covering the femoral head and the surface of the acetabulum always receives components for the formation of new cells, that is, regeneration. This is very important for the formation of this cartilage, because with each movement of the hip it wears out, but usually it is immediately restored. But when injured or under the influence of other factors, this does not happen, which leads to the development of arthrosis of the hip joint, namely the thinning and destruction of its hyaline cartilage.
As a result, deformed areas form in the ideal smooth cartilage, which increases as the pathology progresses. When it is abraded, the surface of the bone that makes up the joint is exposed. When they come in contact, there are features of severe dryness and pain. This triggers the formation of osteophytes and, in the final stages of development, the femoral head is fully fused with the acetabulum, making any movement in the hip joint impossible.
At the same time, arthrosis of the hip joint can trigger the development of various inflammatory processes in the joint, including:
- bursitis - inflammation of the synovial bags;
- tendovaginitis - an inflammatory process in the sheath of the muscle tendons;
- tunnel syndrome - nerve compression, causing pain that radiates along the choked nerve.
The reasons
One of the common causes of the development of arthrosis of the hip joint is mechanical damage, not only direct injury, but also micro damage caused by the damaging effects of excessive load on it. One of the most common causes of disease progression is femoral neck fractures.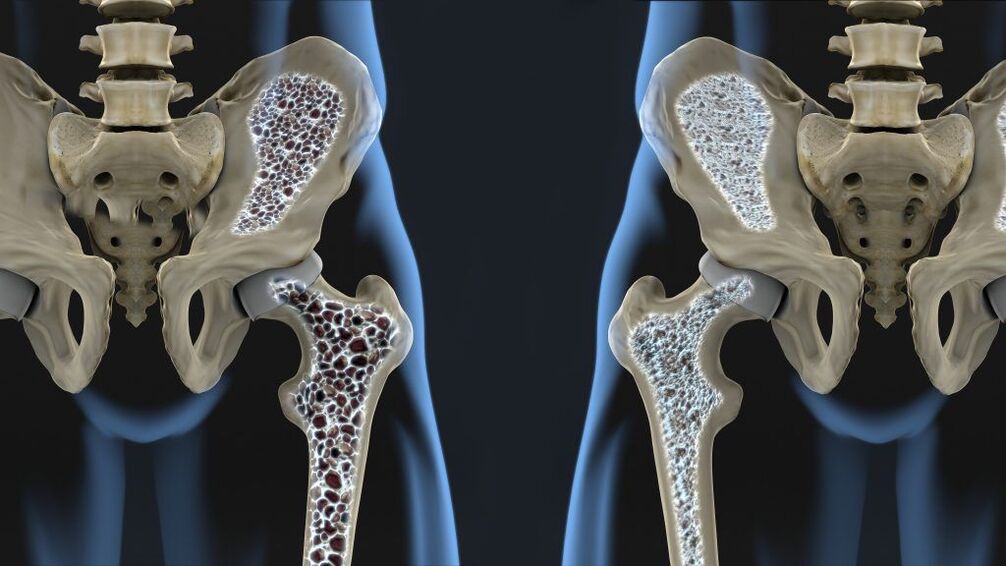 It departs from the femur at a 120 ° angle and connects it to the head. The presence of osteoporosis significantly increases the likelihood of a hip fracture, but such injuries can also be caused by road accidents, falls on your feet from heights, impacts, etc.
It departs from the femur at a 120 ° angle and connects it to the head. The presence of osteoporosis significantly increases the likelihood of a hip fracture, but such injuries can also be caused by road accidents, falls on your feet from heights, impacts, etc.
Fracture of the femoral neck may be accompanied by aseptic necrosis of the femoral head, which will be a trigger for the development of degenerative-dystrophic changes in the joint. The presence of dysplasia or subluxation of the hip joint, rupture of its ligaments, transcondylar fracture or fracture of the acetabulum also creates favorable conditions for damage to its structure. In such situations, arthrosis after trauma of the hip joint is diagnosed.
Often, post -traumatic hip arthrosis occurs in lightweight and professional weightlifters, paratroopers, loaders, and skater.
The development of arthrosis of the hip joint after injury is due to violation of the suitability (comparison) of the articular surface, decreased quality of blood supply to the joint components and prolonged immobilization. As a result of prolonged immobility, not only a deterioration in blood circulation in fixed areas, but also a shortening of muscles, a decrease in their tone. The likelihood of post-traumatic arthrosis increases significantly when inappropriate conditions or untimely treatment are carried out, leading to the preservation of deformities of varying severity. Also, the risk of its development increases with too early loading on the joints and inadequate exercise therapy, including too intense, starting late or otherwise earlier.
Sometimes the disease occurs after surgical intervention on the hip joint due to scar formation and additional tissue trauma. Although in some cases, surgery is the only way to eliminate the consequences of the injury.
Excessive load can also trigger changes in the hip joint, as it leads to microtrauma. Frequent tissue damage activates the process of division of chondrocytes (cartilage tissue cells). This is accompanied by an increase in the intensity of cytokine production, which is usually produced in small quantities. Cytokines are mediators of inflammation, in particular, the cytokine IL-1 leads to the synthesis of certain enzymes that destroy the hyaline cartilage of the hip joint.
In addition, high loads can trigger subchondral plate micro fractures. This leads to gradual compaction and the formation of bone growths on the surface, called osteophytes. They can have sharp edges and cause more damage to the joints, as well as injury to the surrounding tissues.
The subchondral plate is the outermost part of the bone that is in direct contact with the hyaline cartilage.
In some cases, it is not possible to determine exactly what triggers the development of degenerative-dystrophic changes in the hyaline cartilage of the femoral head and acetabulum. In such situations, idiopathic or primary arthrosis of the hip joint is diagnosed.
Today it has been established that the tendency to develop it can be inherited, i. e. the presence of this pathology in close relatives significantly increases the chances of developing arthrosis of the hip joint. Presumably, it has a polygenic inheritance, i. e. its development depends on the presence of many genes. Each of them individually creates mild prerequisites for the development of the disease, but when combined, it becomes a matter of time, especially when leading an inactive lifestyle and obesity, or conversely, hard physical labor.
There is a theory that hip joint arthrosis is the result of a congenital or acquired mutation of the procollagen type II gene.
There is also secondary arthrosis of the hip joint, which develops against the background of the presence of concomitant diseases and age -related changes.
symptoms
The disease is characterized by the occurrence of pain, limited mobility and dryness in the hip joint, the severity of which directly depends on the degree of neglect of pathological changes. In the final stages of development, shortening of the affected leg and complete immobility of the hip joint can be observed, which is due to the complete fusion of the bone structures that make it up.
Initially, the disease can go on without obvious symptoms and cause mild and short-term pain. As a rule, they appear after doing physical exercise, in particular walking, carrying heavy loads, squatting, bending. But when degenerative-dystrophic changes in the joint progress, the pain increases. Over time, they become not only more intense, but also last longer, and the interval between the onset of physical activity and their appearance also decreases. At the same time, rest, even long, may not bring relief. After that, the pain can torment a person even with prolonged immobility of the hip joint, for example, after a night’s sleep.

If the intra-articular structure violates nearby nerves, the pain can spread to the groin, buttocks, thighs and knees. However, they tend to increase with hypothermia. In the last stages of disease development, the pain becomes unbearable. This causes the unconscious desire to feel pity on the foot and reduces pressure on the foot, which leads to lameness.
Another symptom of hip arthrosis is a decrease in range of motion. Often, there are limitations in the ability to turn the legs in and out, to raise the bent leg at the knee to the chest. Over time, what is called morning stiffness occurs, which disappears after the patient "diverges". Thereafter, compensatory curvature of the pelvis is possible, leading to changes in gait. In the future, the patient completely loses the ability to make certain movements with the affected leg.
If arthrosis of both hip joints develops at the same time, a development called duck gait with the pelvis retracted and the body deflected forward is observed.
All this may be accompanied by the formation of edema in the hip joint. But with the presence of excess weight, they can go unnoticed.
Often, during movement, especially extensor, dryness occurs in the affected joint. It is a result of the surface exposure of the femoral skull and acetabulum and their friction with each other. In this case, there is a sharp increase in pain.
Also, with arthrosis of the hip joint, painful femoral muscle spasms can occur. With highly advanced degenerative-dystrophic disease, when the joint space is almost completely lost, and the femoral head begins to flatten, shortening of the affected limb by 1 cm or more is observed.
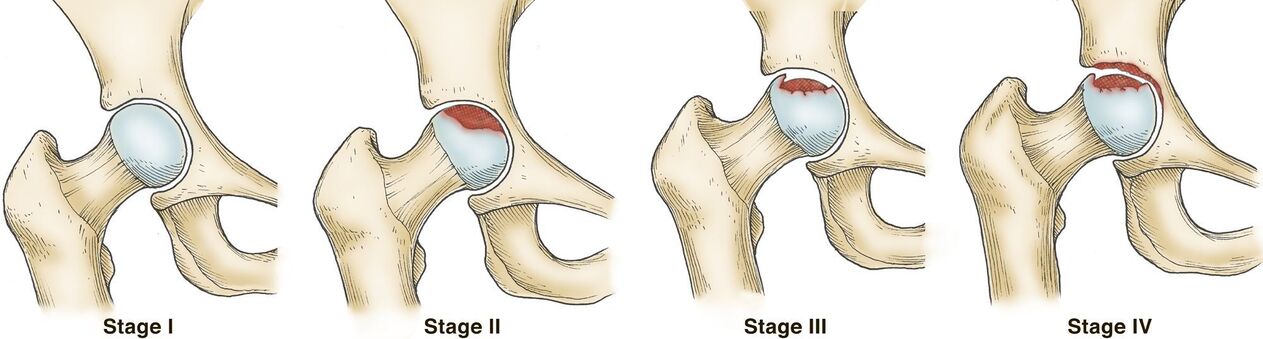
In general, there are 3 degrees of hip arthrosis:
- Grade 1 - the joint space of the hip joint narrows, and the edges of the bone structure are slightly pointed, indicating the beginning of osteophyte formation. Clinically, there is a fairly pronounced pain syndrome and some restriction of movement.
- Grade 2 - joint space is narrowed by more than 50%, but less than 60%. Significant osteophytes were observed, as well as signs of cysts in the bone epiphysis. Patients noted significant limitation of movement in the hip joint, the presence of cramps during movement, pain, and atrophy of the thigh muscles with varying severity could be detected.
- Grade 3 - joint space is reduced by more than 60% or completely absent, and osteophytes occupy large and large -sized surfaces, subchondral cysts are observed. The hip joint is stiff, the pain can be unbearable.
Diagnostics
The appearance of pain and other symptoms characteristic of arthrosis of the hip joint is a reason to contact an orthopedic specialist. The doctor will be able to suspect his presence, especially if he has had a hip or pelvic injury in the past, based on data obtained during interviews and examinations.
The presence of arthrosis of the hip joint is indicated by pain, the intensity of which increases over several years. More rarely, there is a rapid development of degenerative-dystrophic changes, when several months pass from the appearance of the first signs to a strong permanent pain syndrome. This is characterized by increased pain while standing or while doing physical work. Also, for arthrosis, the presence of morning stiffness, which lasts up to half an hour, is typical, and also occurs after prolonged immobility. Gradually, there is an increase in mobility restriction and deformation of the hip joint, which in the final stages of development, an orthopedic specialist may notice during an examination.
However, all patients must be given instrumental research methods, with the possible help of which to confirm the presence of hip arthrosis and determine its degree, as well as to distinguish it from several other diseases accompanied by similar symptoms. As a rule, diagnostics are carried out using:
- Radiography - allows you to detect the main signs of arthrosis, in particular narrowing of the joint space and the presence of osteophytes. But recently, CT has become a more informative research method, making it possible to assess the condition of the hip joint with greater accuracy.
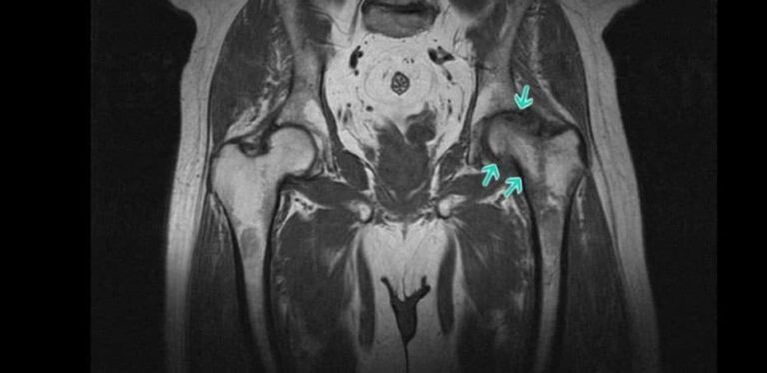
- MRI is a very informative method for diagnosing various changes in the state of soft tissue structure, including cartilage tissue, which makes it possible to detect the slightest sign of hyaline cartilage degeneration.
Also, patients can be prescribed laboratory tests, including KLA, OAM, biochemical blood tests, etc. They are required to establish a corresponding disease that has created a prerequisite for the development of secondary arthrosis of the hip joint.
Treatment of hip arthrosis without surgery
Treatment of degenerative-dystrophic changes in the hip joint through conservative methods of therapy is possible only with stage 1 and 2 arthrosis. Prescribed measures can improve the patient's condition, stop or at least slow the progression of pathology and thus maintain working capacity. But they cannot lead to a complete regression of the changes that have taken place in the joints.
Today, as part of the conservative treatment of hip arthrosis, the following are prescribed:
- drug therapy;
- exercise therapy;
- physiotherapy.
Also, patients are advised to make certain adjustments to their lifestyle. Therefore, in the presence of excess weight, it is necessary to take measures to reduce it, that is, increase the level of physical activity and reconsider the nature of nutrition. If the patient is actively involved in sports and strains the joints, which causes microtrauma in them, it is recommended to reduce the intensity of training.
Medical therapy
Drug therapy for arthrosis of the hip joint is always complex and includes drugs from different groups aimed at reducing the severity of the symptoms of the disease and improving the flow of metabolic and other processes in the joints. To:
- NSAIDs - drugs with anti -inflammatory and analgesic effects, produced in oral form and in the form of local agents, which allow you to choose the most effective and easy -to -use option;
- corticosteroids - drugs that have strong anti -inflammatory properties and are used in most cases in the form of injectable solutions, because when choosing systemic therapy they cause the development of unwanted side effects;
- chondroprotectors - drugs synthesized based on the natural components of cartilage tissue used by the body to restore it (prescribed for a long course);
- muscle relaxants - drugs indicated for muscle spasms, which cause pain of varying severity;
- Vitamin B - helps improve nerve conduction, which is necessary for the development of carpal tunnel syndrome;
- preparations that improve microcirculation - help increase the intensity of blood circulation in the affected area, which leads to an increase in the rate of metabolic processes and helps restore damaged cartilage.
If concomitant disease is detected, consultation of relevant specialists and appropriate treatment is indicated.
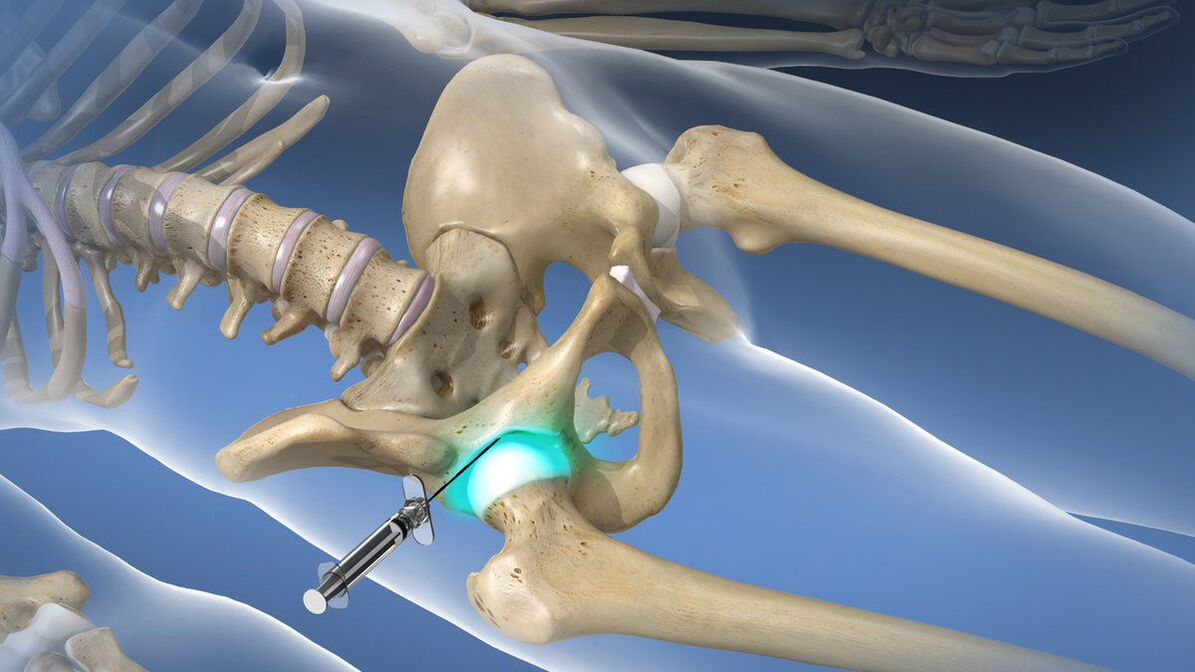
With very strong and debilitating pain syndromes that cannot be eliminated with the help of prescribed NSAIDs, intra-articular or periarticular blockade may be performed. They involve the injection of a local anesthetic in combination with corticosteroids directly into the joint cavity, which quickly leads to an improvement in well -being. But such a procedure can only be performed in a medical institution by a qualified specialist, if there is no high risk of complications.
exercise therapy

Physiotherapy training plays one of the major roles in the non-surgical treatment of hip arthrosis, both idiopathic and post-traumatic forms. But a set of exercises must be selected individually, taking into account the nature of the previous injury, the patient’s level of physical development, and pre -existing comorbidities.
Exercise therapy should be done daily in a comfortable state without haste. All movements should be performed smoothly without jerks, so as not to endanger the already deformed hip joint. This will allow:
- reduce the intensity of the pain syndrome;
- increase joint mobility;
- reduce the risk of muscle atrophy;
- increase the intensity of blood circulation and metabolic processes.
Physiotherapy
To increase the effectiveness of the prescribed measures, it is often recommended that patients with arthrosis of the hip joint undergo a course of physiotherapy procedures. Traditionally, those with anti-inflammatory, anti-edematous and analgesic effects are selected. To:
- ultrasound therapy;
- electrophoresis;
- magnetotherapy;
- laser therapy;
- shock wave therapy, etc.
In some cases, plasmolifting is indicated, that is, the introduction of the patient’s purified blood plasma and its own platelet saturation. To obtain it, venous blood is taken, which is then subjected to centrifugation. As a result, it is divided into a mass of erythrocytes and plasma, which are used to treat degenerative-dystrophic changes in the hip joint.
Surgery for arthrosis of the hip joint
When diagnosing stage 3 hip arthrosis, surgical intervention is indicated for the patient. It can also be done with the ineffectiveness of conservative therapy and persistent pain and restriction of mobility already in the 2nd stage of disease development.
In general, the indications for hip surgery are:
- significant decrease in joint space size;
- the presence of persistent and severe pain;
- significant movement restriction.
The most effective and safe operation for hip arthrosis is arthroplasty. Today it is recognized as the gold standard for the treatment of this pathology, regardless of the cause of its development. The essence of this type of surgical intervention is to replace part of a component of the hip joint or the whole with an artificial endoprosthesis. The prosthesis itself is made of biocompatible and durable material.
Their installation allows you to fully restore the normal mobility of pathologically altered hip joints, relieve pain and give the patient the opportunity to live a full life. For each patient, the type of arthroplasty was selected individually based on the degree of destruction of various joint components.
The most effective is total or total hip arthroplasty. It involves the replacement of the entire joint with an artificial endoprosthesis, i. e. , the acetabulum, the femoral head and its neck. Such prostheses can function without interruption for 15-30 years and ensure full total restoration of joint function.
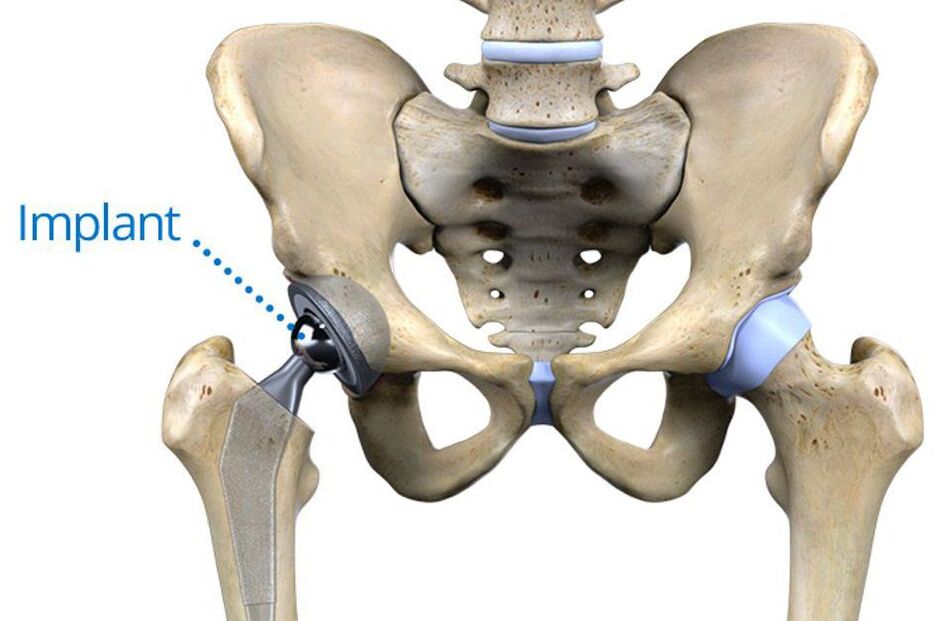
They are installed without cement or with the help of special cement. The first method is more suitable for young patients, as it involves the fixation of a prosthesis in the pelvis by developing into a spongy layer of its own bone in it. For older people, the method of installing an endoprosthesis using cement is more appropriate, which holds the artificial material firmly to the bone surface even in the presence of osteoporosis.
If the normal hyaline cartilage lining the surface of the acetabulum is preserved, the patient may be offered partial arthroplasty. The essence is to replace only the head and neck of the femur with an endoprosthesis. Today, there are 2 types of such structures: monopolar and bipolar.
The first is less reliable; after its installation, it then becomes a requirement for total arthroplasty. This is due to the fact that the replaced artificial femoral head, when making a movement, rubs directly against the cartilage of the acetabulum, which gives rise to its more rapid wear.
Bipolar endoprostheses do not have such disadvantages, because in them the artificial femoral head is already enclosed in a special capsule, which is adjacent to the acetabulum. Thus, the cartilage covering it is not deformed, as the capsule serves as a kind of buffer and artificial substitute for the natural hyaline cartilage of the femoral head.

However, regardless of the type of endoprosthesis performed, postoperative recovery is indicated for all patients. It consists of drug therapy appointments, exercise therapy and therapeutic massage. Recovery time depends on individual characteristics. But it is important to remember that the effectiveness of the operation directly depends on the quality of compliance with the recommendations of the doctor during the recovery period.
Thus, arthrosis of the hip joint is a common disease of the musculoskeletal system, which can occur even in the absence of direct prerequisites for its development. This pathology can lead not only to severe pain, but also to disability, so it is important to diagnose and take steps to stop its progression even at the first signs. However, the current level of medical development makes it possible to overcome advanced cases of arthrosis of the hip joint and restore the full range of motion in it, as well as permanently eliminate severe pain.


















